Author: Leila Shobab
Date: February 2003
The idea of introducing an electric current into your system may seem distressing. However, electrical shock is commonly used to treat patients experiencing heart conditions such as cardiac arrest. Recently, external electrical stimulation has been substituted for gym time and is used to produce "fake" stimulation of the nerves innervating muscles. This often produces the same effects that may result from an (honest) heavy-duty muscular training program. But why would someone carry a battery and some electrodes with him or even implant these devices into his body to receive these electrical stimulations?
One major reason may be to treat the consequences of spinal cord injuries (SCI). SCI can drastically change people's lives; the psychological and socialc impact of such injuries is often devastating. Some of the general disabling conditions associated with SCI are permanent paralysis of the limbs, chronic pain, muscular atrophy, loss of voluntary control over bladder and bowel, inability to produce erection, ejaculation and infertility. The consequences of SCI depend on the specific nature of the injury and its location along the spinal cord.
Bladder dysfunction associated with spinal cord injuries
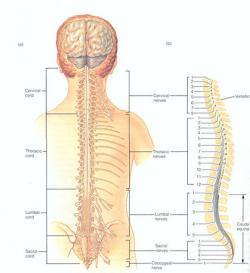
Figure 1 - Spinal cord showing the divisions and specific nerves coming out of each divisions. Courtesy of Gerard J. Tortora (1999) Principles of Human Anatomy (eight edition) John Willy & Sons Inc. , New York
The loss of genitourinary function - the dysfunction of the genital and urinary organs - is one of the most important results of SCI. Specifically, neurogenic bladder, often associated with SCI, results from damage to the nerves controlling bladder function. A lesion above the sacral level (see Figure 1) of the spinal cord, which may or may not involve the brain, could affect how the bladder stores and empties urine. These upper motor lesions are most commonly seen after cerebrovascular accidents (stroke), spinal cord injuries, neurological diseases such as multiple sclerosis, and also infections.
Until recently, the main consequences of spinal cord injury were confinement to a wheelchair and a lifetime of medical help. Treatment options for SCI used to be limited; the available care was highly unsatisfactory and frustrating due to its limited success, unwanted side effects and high costs. However, this has changed since recent advances in neuroscience have drawn considerable attention to research into SCI and have made significantly better treatment and rehabilitation options available.
Understanding electrical stimulation as treatment option
Functional electrical stimulation (FES) is one exciting new treatment option that has shown the potential to enhance nerve regeneration and allow significant improvements in restoring and improving functional capacity after SCI.
Also, in treatment of neurogenic bladder the use of electrical stimulation has seen great advances. However, in order to consider electrical stimulation as a treatment option for neurogenic bladder, the peripheral nerves surrounding the bladder and urethral muscles must still be intact, even though there may be damage to the central nerves at the spinal cord levels.
In FES, electrical stimulation is applied to the surviving neurons using an implanted stimulator which causes muscle contractions. Electrical stimulation is mainly delivered to the sacral anterior nerves coming out of the sacral region of the spinal cord (see Figure 1 and 2)
Figure 2 - Spinal cord connection of nerves to muscle groups of the human body Courtesy of Gerard J. Tortora (1999) Principles of Human Anatomy (eight edition) John Willy & Sons Inc. , New York
To understand how external electrical stimulation can be used to treat neurogenic bladder it is useful to know how stimulation takes advantage of how the nerves on the bladder are structured to ensure bladder function.
The coordinated action of bladder muscles, also known as detrusor muscles, and external and internal sphincters are essential to the process of urination. In order to urinate, the detrusor muscles must contract, while muscles of the external and internal sphincters are relaxed to allow the outflow of the urine (see Figure 3).
The neurons innervating the smooth muscles of the detrusor and the internal sphincter are mainly under involuntary control of the autonomic nervous system, whereas the neural activity at the skeletal muscles of the external sphincter is monitored by the voluntary control of the somatic nervous system versus the autonomic nervous system regulates involuntary actions of the smooth muscles, heart and glands.
The two divisions of the autonomic nervous system are the sympathetic and parasympathetic nervous systems. The nerves of the sympathetic nervous system originates in the thoracic and lumbar regions of the spinal cord and are often recruited during stress situations, such as fear, excitement, vigorous physical activity, etc. The sympathetic nervous system tends to reduce digestive secretion, speed up the heart rate, dilate the pupils and enhance contraction of the smooth muscles along the blood vessels, decreasing blood vessel diameter and increasing blood pressure.
Figure 3 - Structure of the bladder Courtesy of Gerard J. Tortora (1999) Principles of Human Anatomy (eight edition) John Willy & Sons Inc. , New York
A branch of the sympathetic nervous system originating from T11-T12 (see Figure 1 and 2) and mainly innervating the bladder neck increases bladder storage capacity. Damage to this branch often results in urinary incontinence - the inability to store urine and lack of voluntary control over the loss of the urine. In infants less than 2 years old, urinary incontinence is normal because the neurons to the external urethral sphincter are not fully developed to allow voluntary contraction of the sphincter.
The parasympathetic nervous system originates in the brain stem and lower part of the spinal cord. In general, this system inhibits or opposes the physiological effects of the sympathetic nervous system, intending to stimulate digestive secretion, slow down the heart rate, constrict the pupils and dilate blood vessels.
A branch of the parasympathetic nerve supply originates from the sacral cord at S2-S4 (see Figure 1 and 2) and travels to the bladder, governing the contraction of the smooth muscles of the detrusor. Activation of this branch of parasympathetic nerve promotes bladder emptying. Damage to this branch often leads to urinary retention - the inability to empty the bladder.
Spinal cord injuries can affect the parasympathetic supply to the detrusor muscles or the sympathetic supply to the bladder neck as well as somatic nerve supply to the external urethral sphincter.
Application of functional electrical stimulation to bladder dysfunction
In the application of FES to treat neurogenic bladder, electrical stimulation is delivered to the sacral anterior roots to induce bladder contraction for bladder emptying. The electrical stimulation causes activation of small non-myelinated efferent parasympathetic nerve fibers, directly inducing contraction of detrusor smooth muscles, which leads to evacuation of the bladder.
Currently, sacral nerve roots stimulation is clinically used in combination with complete sacral deafferentation, the complete surgical trans-section of all afferent nerve roots providing sensory input from the detrusor muscles to the sacral segments S2-S4 of the spinal cord.
In this way, the sensory stimuli from the detrusor muscles cannot reach the central nervous system, and consequently, reflex activities generated by the central nervous system causing uncontrolled bladder contractions can be inhibited. This procedure is also termed posterior phizotomy. The procedure is necessary to prevent reflex activities of detrusor muscles and allows large amount of urine to be stored at low bladder pressure.
An approach to inhibit reflex activities of detrusor muscles has been investigated by some researchers using capsaicin, the pungent extract from red pepper.
"Capsaicin exerts a selective action on certain sensory nerves, most notably those involved in reflex contractions of the bladder after spinal cord injury," says Victor W. Nitti from the State University of New York Health Science Center at Brooklyn.
In a commentary in the November 6, 1994 issue of the Lancet, Nitti implies that after acute application of capsaicin to these nerves, there is excitatory action. However, after exposure to a high dose, the sensory nerves become desensitized to capsaicin as well as to natural stimuli. Desensitization as well as posterior rhizotomy involves blocking at the afferent level. Posterior rhizotomy, however, results in a permanent paralysis of the muscles involved as opposed to the relatively temporary effect of capsaicin.
The Brindley bladder stimulator
Based on experimental work in baboons, G.S. Brindley approached the problem by developing a stimulation system using electrodes, placed on the bilateral S2-S4 sacral anterior nerve roots. The Brindley Vocare Bladder System is now used in combination with posterior rhizotomy and has shown good results in management of neurogenic dysfunction of the bladder.
"The Brindley bladder stimulator delivers intermittent stimulation to the anterior sacral roots," report H.E. van der Aa H.E. and colleagues.
"The stimulus parameters can be adjusted and set specifically for individual use. Its primary purpose is to improve bladder emptying, thereby to eliminate urinary infection and to preserve kidney function. It also assists in defecation and enables male patients to have a sustained full erection."
The Brindley Bladder System consists of four main components: The external RF-Control Unit: This unit is the only part that is placed externally. The unit sends radio waves across the surface of the skin to the stimulator that is implanted inside the abdominal cavity.
There are three primary control options to manipulate urination, defecation, and to produce erection when needed.
Surgically implanted Receiver-Stimulator: This component is implanted in the abdominal area. The stimulator receives the radio frequency stimulation from the transmitter and generates electrical impulses that are conducted through the leads to the electrodes and then to the nerves controlling bladder function. Surgically implanted leads: Leads or wires are used to conduct the electrical impulses from the stimulator to the electrodes attached to the nerves. The wires are about 50 cm long. Surgically implanted electrodes: Electrodes are mostly made of silicone and soft conductors fabricated in a way to reduce trauma and compression of the nerve. The most common type of electrodes is cuff-like and is placed around the specific nerves that need to be stimulated. The average length for the electrodes used to stimulate bladder nerves is 1-2 cm.
A major challenge in the use of external electrical current to establish controlled urination is the differential responses of the bladder muscles and the uretheral sphinter muscles to these stimulations.
"In the past, efforts to restore bladder control using electrical stimulation have been unsuccessful due to the fact that nerve roots that supply the sphincter muscles and the bladder muscles contract simultaneously upon electrical stimulation, thereby counter acting each other," said Brindley in 1986 and 1991 reports.
In comparison to the nerves innervating the bladder, the neurons to the external sphincter muscles have a lower threshold to produce action potentials that generate muscle contraction. This means whenever electrical current is utilized to produce contraction of the bladder muscles (detrusor muscles), the muscles of the external sphincter are also stimulated, and then contraction of these muscles prevents the outflow of the urine.
To allow the outflow of urine, the external sphincter muscles must relax completely while the bladder muscles are contracting, to 'force' the volume of urine from the internal cavity. If the sphincter is not allowed to relax, not only can urine not exit the bladder, but dangerously high pressure may result inside the bladder that could lead to serious and irreversible damage to the kidneys.
Fortunately, researchers have established a trick to use electric current to stimulate the bladder muscles and at the same time allow relaxation of the sphincter muscles. The muscle fibers that constitute the sphincter are mainly "fast twitch" muscle fibers, producing relatively high amounts of force, but also fatigue easily and relax very quickly. In contrast, the fibers that compose the detrusor muscles are "slow twitch" and initiate contraction quite gradually and have the capacity to maintain force for a longer period of time without becoming fatigued. The trick is to deliver short bursts of high frequency electrical pulses generated by the stimulator to the sacral nerve root that is coming out of the spinal cord at the sacral regions and is innervating most of the muscles involved in the urinary system.
Intermittent stimulation bursts to the anterior sacral roots can be timed in a way that the peaks of contraction of the sphincter and bladder are out of phase; the contraction of the two don't occur at the same time.While the sphincter relaxes rapidly at the end of each stimulus burst, the pressure in the bladder is still sufficiently high to produce urination.
In more simple words, after the pulses reach the urinary system, the first fibers that are stimulated to contract are the muscle fibers of the sphincter. Yet they are also the ones to relax first while the muscle fibers of the bladder are still in the state of contraction. This allows the outflow of urine in between the bursts of stimulation. The Brindley bladder stimulator takes advantage of this differential contraction and relaxation characteristics of the sphincter and bladder wall muscles. Using this method has enabled patients with loss of voluntary bladder control to utilize electric stimulation effectively to regain significant control over their bladder function.
Special Considerations
Not all patients with spinal cord injury qualify for this implant system. Patients must have established skeletal maturity, because if the body is still growing, the electrodes may be displaced and the entire system may not be stable. Also, to qualify for FES treatment, a complete lesion of the spinal cord must be established. If the lesion of the spinal cord is incomplete or partial, some of the nerves still have a chance to regenerate and regain function, which may eliminate the need for artificial stimulants. The patient must also be in a neurologically stable condition in order to manipulate the Brindley device and establish the right time to utilize it. Additionally, the peripheral nerves found in the bladder and sphincter muscles must be intact to respond to exogenous electrical stimulations. Some considerations regarding the use of Brindley Bladder System may include infection during the surgery, leakage of cerebrospinal fluid along the cables that may form a swelling around the receiver block, changes in defecation pattern, and constipation if the implant is not used.
Electrical stimulation of the sacral nerve using Brindley Bladder system has made an enormous contribution to the treatment methods available for treating neurogenic bladder problems in patients with a complete spinal cord lesion. The great advances to date allow us to look optimistically toward the future and hope for even greater improvements and achievements in treating neurogenic bladder.
Glossary of Terms
Autonomic Nervous System (ANS) - also known as 'visceral nervous system', is a division of the nervous system important for regulation individual organ function and homeostasis. In most situations, we are unaware of the workings of the ANS because it functions in an involuntary, reflexive manner. For example, we do not notice when blood vessels change size or when our heart beats faster. Capsaicin - a colorless, pungent, crystalline compound, C18H27NO3. Derived from hot peppers of the genus Capsicum, including chili, cayenne, and jalapeno, and responsible for the hotness of those peppers. It is a cytotoxic alkaloid, often causes pain, irritation, and inflammation, and is mainly used to study the physiology of pain and gastrointestinal stimulation. Chemical name:
6-Nonenamide, N-((4-hydroxy-3-methoxyphenyl)methyl)-8-methyl.
Cerebrospinal Fluid (CSF) - a clear liquid circulating through the ventricles of the brain, spaces around the brain, and spinal cord, which is very similar to the liquid portion of blood (plasma) and contains various compounds such as sodium, calcium, bicarbonate, chloride, magnesium, and glucose. CSF is used as a medium for the transport of chemicals to and from the brain, and to provide buoyancy and protection to the brain. Detrusor muscle - a collective name for the muscles making up the middle layer of the bladder wall. The inner layer of the bladder wall is called mucosa (important for secretion of mucus) and the outer layer, called adventitia, consists of a sheath of connective tissue. Detrusor muscle, in between the outer and the inner layers of the bladder coats, consists of three layers of smooth muscle fibers: inner longitudinal, middle circular, and outer longitudinal. These muscles are under involuntary control of the nervous system. In order to urinate, the detrusor muscles must contract to expel the volume of urine out of the bladder. Myelin - a white fatty material, composed chiefly of lipids and lipoproteins, enclosing certain axons and nerve fibers. The main function of myelin is to increase the velocity of stimulus conduction in nerve fibers. Non-myelinated nerve fibers are generally smaller and conduct electrical impulses slower. Generally, nerve fibers transmitting tactile stimulus to the central nervous system are relatively larger and are myelinated, whereas nerve fibers conducting pain from various parts of the body to the central nervous system are non-myelinated or thinly myelinated and consequently conduct painful stimulations at a much slower rate. This may be the reason why, when you step on a sharp object, you first withdraw your foot before saying "ouch." Neurogenic - arising from or caused by the nervous system, for example neurogenic disorers, neurogenic tumors and neurogenic bladder (where the dysfunction is caused by a damage to the nerves controlling the bladder function). Posterior Rhizotomy refers to the surgical procedure during which sensory nerve rootlets that come from the muscles (e.g., bladder muscles, lower limbs) and enter the spinal cord are selectively sectioned (i.e. cut). The procedure is used to avoid reflex contraction of the bladder muscles (which may otherwise lead to uncontrolled bladder emptying) and reduce spasticity in the lower limbs after cerebral palsy or spinal cord injury.
For more information, visit: http://cerebralpalsy.wustl.edu/rhizotomy0.html
Somatic Nervous System (SNS) consists of peripheral nerve fibers that send sensory information from the sensory receptors to the central nervous system and motor nerve fibers that project to skeletal muscles. The activities of the somatic nervous system are under voluntary control. Sphincter - The internal and external sphincter muscles form a ring around the urethra (the small tube through which urine flows from the bladder and empties from the body) to keep urine in the bladder. The external sphincter can be controlled voluntarily, whereas the contraction and relaxation of the internal sphincter is involuntary. In order to urinate, both the external and internal sphincters much be relaxed so that urine is able to flow through the urethra and exit the body.
For further information, visit: http://depts.washington.edu/rehab/resources/bladder.shtml
Urinary incontinence is the inability to control urination. It may be temporary or permanent and can result from a variety of problems in the urinary tract. Urinary incontinence is generally divided into four groups according to the malfunction involved: stress, urge, overflow, and functional incontinence. Often, more than one type of incontinence is present. The condition itself is a symptom rather than a distinct disease, and this is one reason why it is difficult to determine a definite cause. Urinary retention is characterized by the inability to empty the bladder completely or at all. People with this condition often must resort to using a catheter to empty their bladder. Complications associated with this condition can include urinary tract infections and kidney damage.
Suggested Reading
Benevento BT, Sipski ML (2002): Neurogenic Bladder, Neurogenic Bowel, and Sexual Dysfunction in People With Spinal Cord Injury. Physical Therapy; 82-6: 601-12
Brindley GS (1986): Sacral root and hypogastric plexus stimulators and what these models tell us about autonomic actions on the bladder and urethra. Slin Sci 70: 41s-44s
Brindley GS (1991): The Finetech-Brindley bladder controller: notes for surgeons and physicians. Finetech, Welwyn Garden City
International Continence Society 2002
http://www.icsoffice.org/publications/2002/pdf/tnu.pdf [Link current as of February 1, 2002]
Van der Aa HE et al. (1999) Sacral Anterior Root Stimulation for Bladder Control: Clinical Results. Archives of Physiology and Biochemistry; 10703: 248-56
Tortora GJ. (1999) Principles of Human Anatomy (8th ed.). John Wiley & Sons, Inc. New York.
Nitti VW. (1994) Intravesical Capsaicin for Treatment of Neurogenic Bladder. Lancet; 00995255, Vol. 343, Issue 8911.